Form and light in the public library.
Hope you have a good weekend everybody!
Your Custom Text Here

Photo Credit: Marisa Farnsworth
Form and light in the public library.
Hope you have a good weekend everybody!
I wanted to share these thoughts to help people understand what mental illness really means.
I've been sick with schizophrenia since I was 18 and I'm 54 now. Mental illness can be deadly and is little understood in the world today (still). As a patient, I had to learn about my own illness in order to move forward with my life. People without mental health challenges need to learn about mental illness, too. We can't stay in the Dark Ages forever.
Everyday I hear someone say, "so and so is nuts/crazy/a lunatic" in an attempt to describe behavior they find offensive and contradictory to what they believe. Please refrain from attaching "insane" to evil or wrong behavior/beliefs. It makes you sound uninformed at best and unintelligent as well. We are sick, not evil. Thank you.
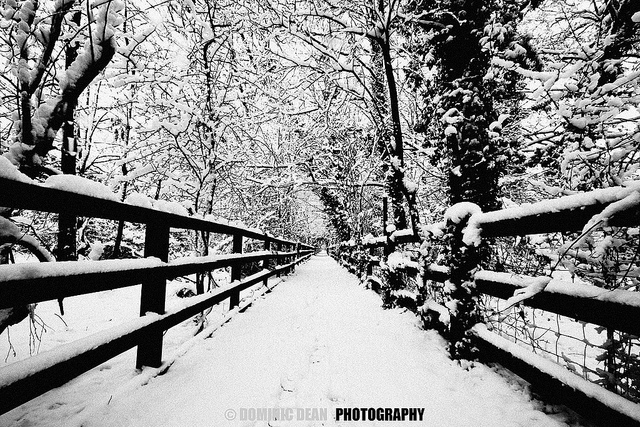
Photo Credit: Dominic Dean
Flickr
“I can’t live here, Grandma. Thousands of spiders come out of the vent in the bathroom.” Just another day with a challenge for me.
I’d tried to put AJ into an apartment nearby to see how he’d handle being a bit on his own. Still, there was the need to go clean and feed him as these were not things he would do for himself.
AJ had a childhood history of being “different”. There were many diagnoses from a very early age — ADHD (Attention Deficit Hyperactivity Disorder), OCD (Obsessive Compulsive Disorder), ODD (Oppositional Defiant Disorder) and 15 other labels. AJ attended a special-needs school which was the only option at the time and a long commute. A school that held juvenile delinquents, and anyone who made the public school teaching difficult, was no solution for someone who spent most of the time in a fetal position under his desk or in the padded room that increased his anxiety.
At 17, AJ entered a private institution because it was believed it could help him. The trauma he experienced at the hands of staff specialists was brutal and pushed what may have been moderate schizophrenia into extreme illness. He suffered forced medications and blood work while being tied down, a shaved head, straight-jackets, and no visitations — things you would see in old horror movies.
When he was 18, a social worker asked me if I would take AJ. She told me to grieve my grandson’s death as the person I once knew was gone forever. After many classes on what to expect, AJ came to live with me in my belief that love could make this better. Of course, I’d take him. It was a privilege — I’d loved him before he was even a twinkle in his young mother’s eye.
There was a short honeymoon period when behavior wasn’t frightening but, as time went on, it became clear AJ’s mind was more tortured than I ever thought possible. In the first years he lived with me I tried to teach him to cook — he was afraid to even stand by the stove. He refused to shower or change clothes. He wrapped his legs with chains. He rarely spoke. There were many different personalities to deal with. Hopes for a normal life dwindled. While I was driving him one day and had to stop at a light, he insisted I proceed as there was no car crossing our path. That was the day I realized he should never be encouraged to drive. And when demons came and went uncontrollably, there’d be damage to property, thoughts of death, and letters of dying and darkness.
As I grew older, I needed to know if AJ could live on his own with some help. That’s where the apartment idea came in. And by the time I moved him to one, I’d found ways to handle the monsters in the walls and the spiders in the vents. After all, why couldn’t there be a special spray that would kill monsters and spiders forever?
I couldn’t find solutions for everything, though, and eventually AJ returned to live with me. The days were never normal. A few minutes at a time were okay but I couldn’t leave him alone for more than an hour or two. I lived through painful moments trying to decide if it was time for a 5150 (72-hour involuntary hold) knowing that he would be triaged out as he answered the all-important question: “Are you a danger to yourself or others?” Everyone in the triage area knew how to answer that. There were a few times when a 5150 held and became a 5250 or longer stay but medications always included terrible side-effects.
For AJ, days and nights exist when his tortured mind begs for someone to end his misery. He spends hours telling me he doesn’t want to be a burden even though I try to reassure him I’ll always be there for him. And sometimes he warns me to leave the house until his violent thoughts can calm down.
For me, I fill many nights with tears knowing about my grandson’s tormented brain. And there’s pain, much pain from family and friends who advise, “Put him in an institution or make him homeless.” For years, I’ve tried to educate these people that there are no institutions for him; no homes that can house his extreme condition. Now, I ask them to give me a phone number to call knowing there is no phone number to call. I watch the expressions on their faces because this is not the reaction they were expecting. They were expecting me to agree and say, “Yes, I’ll put him in an institution.” There are no appropriate facilities and I know they won’t try to help me find one.
Until you experience the disease, until it affects you and you’ve come to grips with the lack of care and resources available, until you’re scared enough to do the research, you’re ignorant of the situation. I wonder why others don’t thank caregivers for keeping the rest of the family, neighbors, and world safe by watching over and caring for these extremely ill people?
This is my beloved grandson. My heart embraces him. I’m committed to be there for him as long as I’m able to care for him. And I fear for his future when that day ends.

Maggie

Photo Credit: Marisa Farnsworth
"Lucky me. I got a room with a view."
Hope you have a good weekend everybody!
Sis Kaya Tama IsesaJah-Bell recently identified ten myths that mental health providers tell family members. GG Burns, brain health advocate, simplified Tama's words into this poster/meme and added an etching Joann Strunk made of her daughter. The image is shattered which is how parents and family members feel when the system breaks down and kills children and loved ones. As mental health advocate Teresa Pasquini writes, "We must tell our stories to #shattershame. Families & caregivers all have to get comfortable with being uncomfortable about the current state of the mental health care system. We must refuse to be silent and allow harm."


Debra
I hurry into the inpatient psychiatric unit just in time to wait. It's smoke time on the patio. The nurse hands me a stack of charts representing residents in need of an assessment.
”Who is ready?” I ask.
She looks as if my brain misfired. “Everyone on the unit is smoking.”
It's been years since I visited my own loved one in the psychiatric hospital, but I still remember the loud clanking of the key as it enters the lock. The noise is deafening to one who painfully wishes their loved one is anywhere but here. Patients approach to ask if they can leave for our facility where there are no locks. There is much to learn from someone in the allocated twenty minutes. At the end of the day, there are 12 patients who appear ready to return to community living.
I exit the locked door which opens to the waiting room. Tired, I find a chair by the window and fall into it. A few minutes pass and then I see them. A familiar knot forms in my stomach reminding me of my own feelings of hopelessness in years gone by. Confusion and the nervous sensation when, a lifetime ago, I searched for the right thing to do for my loved one with mental illness.
Jolted into the present, I see staff lead a young man out to visit his waiting parents. The parents look in their fifties. Their grown son chooses to sit apart alienating himself from those whose hearts are visibly breaking. Where is the look which conveys that I love you and I remember you as Mom and Dad? His legs twitch incessantly and the rhythm of anxious fingers scrape the hollow of his neck. He never returns eye contact as his parents search for any hint of connection. The deafening silence - I've heard it all before.
“Son, did your day go okay?” The father is wearing a laborer's cap. He appears fragile as if all hope rests on his son’s response.
“Nope.” He averts their gaze. He wears a cross around his neck.
“Please, dear, come over here. You are trembling,” his mother whispers.
She starts to cry. Her fear takes me back to a time when I, too, searched for some feeling or expression from the man I loved. Our shared pain becomes palpable. “Your father and I miss you.”
Then the clamor of the metal key in the lock interrupts the silence. The door swings open. “Smoke time.” The father reaches forward to graze his child’s arm as his son bolts out the door. Mom and Dad look as if they've lost their last friend. It hurts to wear your heart on your sleeve. I know this to be true.
Moments pass. I see it again. The look is unmistakable. I met it, too, with the same sober presence, vigilance, and glassy-eyed turmoil. We feel alone in the battle with mental illness. They lower their bodies into a measured collapse. I want to tell them the emotional disconnect, a part of this illness, can improve. Recovery with medications and therapies is possible yet mental illness is complex.
Our invisible connection prompts one more look. I want to offer a promise of hope and understanding of the life they now live. Instead, I make eye contact and try to smile in support. As much for myself as for them.

Photo Credit: Marisa Farnsworth
Intersection.
Hope you have a good weekend everybody!

Deborah's son, James, and her grandson, Sean Michael.
My son suffers from bio-neurological brain disorders. Without the right treatment and support, his medical condition prevents him from realizing that he has a serious illness. The untreated symptoms of his brain disorders control his thoughts and his actions. His untreated symptoms also control our lives.
My son has schizophrenia, anosognosia (in laymen’s terms, "lack of insight" or "lack of awareness" that he is ill), a history of Capgras Syndrome, a history of command hallucinations, and PTSD.
So what does all this translate into? A preventable tragedy that was almost impossible preventing.
What are our numbers? 1:6. That’s our family’s conservative ratio.
Now what does this ratio mean? It means that my son represents the one (1) who is suffering from his illnesses. The six (6) are the other people in our family who are directly connected to him.
Our lives have been significantly affected by his untreated or treatment resistant medical illness. We live with constant emotional stress from the daily trauma and drama of his severe symptoms — including psychosis and crisis evaluation teams. We experience situational mental illness, like depression or PTSD, due to the hopelessness and isolation of caring for someone with a severe brain disorder when they're not being properly treated and their symptoms are not under control.
We've lost wages from jobs we've had to give up to care for our loved one and from having to move from one place to another due to stigma. We've missed chances of advancement at work and taken lower paying positions in order to be available to meet the needs of our son. We've faced family stress that could lead to divorce and further financial and mental decline of the entire family.
It means that my son’s illness has affected more than just him. It's also impacted his school system, our local sheriff’s department, the juvenile courts, and our relatives who helped provide financial aid to get him on the ‘fast track’ to treatment.
His illness dictated his and our lives — how we spent our time, our money, and our emotional resources. There was nothing left over for our needs. We were all consumed trying to save him, but we're among the lucky ones. In spite of the odds against us, our family stuck together and did what we needed to do to secure his compliance to the right treatment.
What was the cost for his intervention and treatment? Here is a start at some of our other numbers:
Lost wages: I quit my job at DreamWorks and later at Disney on a union job that paid me $70,000 a year with full benefits. I was the only one who could care for my son.
Mental Health: I didn’t have any. I lived in constant high stress of being attacked and threatened by my son along with the stress from the fear of losing him, and the stress of not being able to find timely treatment for him. I paid not only with money, but with my mental and physical health.
Probate Conservatorship: $6,000.
One month in a dual-diagnosis facility before his SSI started up: $6,000.
Qualified therapist who didn’t take insurance: $160.00 per hour once a week.
Equine therapy which worked the best from all the therapies we tried: $160.00 per session per week.
‘Fast Track' — by-passing the waiting list for medical recipients and getting into an outpatient treatment facility that held the most promising form of treatment but didn’t accept our insurance: $250.00 per appointment for two years until, finally, they accepted our son's Medi-Cal.
Blood monitor company: $150.00 per month. We’re going on our seventh year now.
Licensed nutritionalist: $120.00 per visit.
Independent blood test for mercury and other toxins: $180.00.
The list goes on and on. Our son's been in therapy since second grade to work with the behavior we were trying to deal with daily.
We spent and lost thousands of dollars. We have little retirement saved and my husband and I are 57. It was worth every penny and every sacrifice. When we look at and enjoy our son today, there's no price we can put on his life or on how close we all are now.
The problem is, why should we have to pay such a high price for medical treatment for our son? What about the families who don't have the resources we did to secure early intervention and compliance to treatment? What happens to them? What are their numbers? How much worth can you give to a life?
What if my son decides to be noncompliant in the future? What would our fate be then? All this affects and still concerns my whole family. My son’s illness isn’t just his illness. It’s a 1:6 ratio in our family. I’m not counting my brother’s suicide at 15 or my mother’s issues and how they impacted us.
What are your numbers?
There are no statistics that include family numbers in their studies. We're the ones they don’t know about or talk about. We're more invisible than the ones we advocate for. It’s up to us to unify and speak out in one voice for what we need — for our rights to get appropriate treatment for our loved one's medical condition.
It’s their illness but It affects us all.
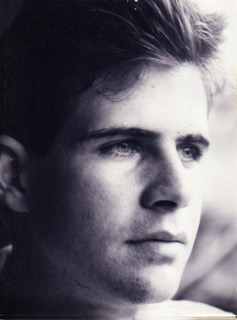
Paul as a young man
What do I do to protect my son, Paul Michael Muskine?
California state medical facilities seem to be doing a good job of evaluating, diagnosing, and caring for mentally ill people. From my experience, Sacramento County people are the opposite - not good at evaluating, diagnosing, or caring for mentally ill people. Why is there so much difference?
My son Paul's been locked up for 1 year and 18 months. He's now at the California Department of Corrections and Rehabilitation in Vacaville where he's diagnosed as severely mentally ill. This is not new. Paul was diagnosed many years ago as severely mental ill. Sacramento Mental Health Court dismissed Paul because of his illness but the public defender, the DA, and the judge sent him to prison when he was not balanced to stand trial and was denied his right to a trial.
In the case against him, I believe Paul was the victim. A drug dealer, who was 6 feet tall and 200 pounds, attacked him. Paul, 5 feet 7 inches tall and 108 pounds, was not the attacker. He was defending himself. I'd do the same thing if I were in that situation.
Turning Point, receiving Prop 63 funds to be Paul's mental health care provider, left him in a rundown motel populated with drug dealers. From his room, Paul had no access to a kitchen. I'd take him shopping and he'd buy two pieces of chicken. He'd cook one piece in a broken down electric pan and store the other piece in a plastic bag in a basket on the floor. The mice would eat the chicken. When I told Turning Point, they said, “We'll get Paul a table and chair." They got Paul a table and a chair and left him in the same situation. He lost 57 pounds.
What do I do to protect my son, Paul Michael Muskine?

Paul today

Photo Credit: Marisa Farnsworth
After the rain...
Hope you have a good weekend everybody!