Three people have forwarded this article to me. Heather Knight is a journalist who often writes about mental illness.
MENTALLY ILL PEOPLE IN SAN FRANCISCO ARE CYCLING IN AND OUT OF EMERGENCY GOOMS. ONE DOCTOR SHARES STORIES ABOUT OUR BROKEN SYSTEM.
Mentally ill people in S.F. are cycling in and out of emergency rooms. One doctor shares stories about our broken system
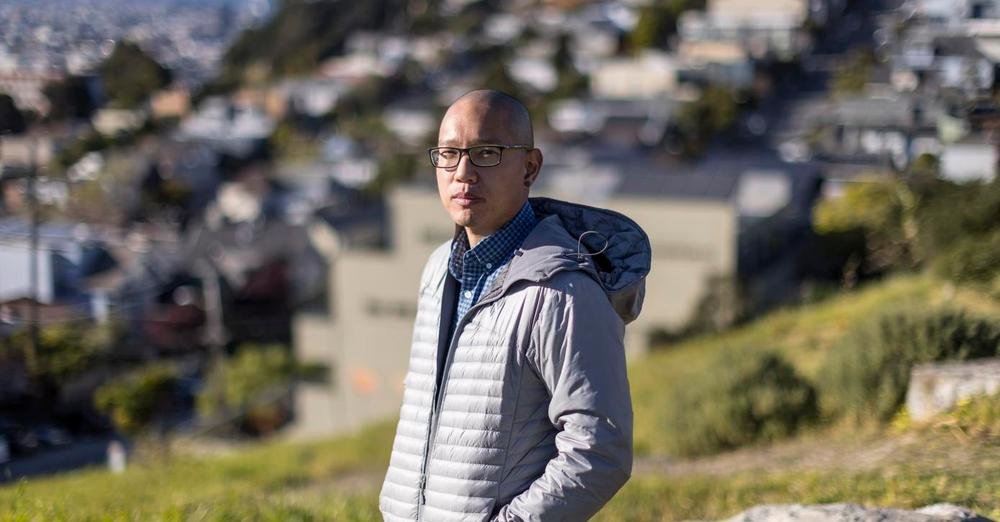
Dr. Scott Tcheng will never forget some of the people who come to his San Francisco emergency room in desperate need of help.
One man who arrived by ambulance looked like the Joker, his face and hands covered in animal blood. A 911 caller had spotted him eating a raccoon crushed by a car on a city street.
Tcheng has treated patients high on methamphetamines who are convinced a mouse is crawling inside their body or that someone has cut off their genitals with a sword.
One person on meth was treated after trying to steal a parked ambulance — with a patient inside. Another tried to captain the Pampanito, the floating submarine museum at Fisherman’s Wharf, but fell into the bay. He had hypothermia by the time a rescue team fished him out.
Just the other day, Tcheng treated a 31-year-old woman who is homeless, suffers from schizophrenia and has come to the ER about 150 times — usually to request pregnancy tests, but sometimes just for food and a place to sleep. This time, the pregnancy test came back positive, but the woman refused offers of hotel vouchers or a shelter bed. So the hospital released her back to the streets.
Other patients suffering from severe, untreated mental illness or meth-fueled psychosis have become violent toward hospital staffers, wrecked medical equipment, brandished knives and hurled their own feces. Some return to the ER shockingly often. Tcheng said one of his patients has visited emergency rooms around San Francisco hundreds of times in the past year.
What unites these patients, beyond their struggles, is their clear need for long-term care. But they’re usually not getting it. Not even in a rich city and a rich state that claim to be compassionate and caring.
The patients are often too sick to accept care. And frequently, there isn’t enough care, or adequate services, to meet their needs. Tcheng must send them back into the world, untethered, until the next ER visit.
“It’s so important that the people of San Francisco know about this,” Tcheng said, explaining his decision to go public about his patients. “They walk by it every day on Market Street and in SoMa, but the average San Franciscan doesn’t realize how deep it goes.”
Tcheng said he’s “cautiously optimistic” that a sweeping new proposal from Gov. Gavin Newsom could make a difference.
Called CARE Court, Newsom’s plan would require every county to provide needed treatment for people suffering from psychosis, whether due to mental illness or drug addiction, and would mandate that patients accept the help. Patients could be brought to the civil court because they allegedly committed a crime, because their involuntary psychiatric hold is ending or because they’re deteriorating on the streets.
If they don’t comply with a court-ordered treatment plan, a judge could turn them over to the regular criminal system, order additional involuntary holds or move toward conservatorship.
Newsom’s proposal suggests he has learned lessons since his time as mayor, when he dealt with recession-fueled budget cuts in part by slashing the number of psychiatric beds at San Francisco General Hospital. A dire bed shortage remains all these years later. He also cut beds in homeless shelters and closed drop-in centers where people could get help during the day.
San Francisco General Hospital is now the only hospital in the city with a dedicated psychiatric emergency room, but there are far more people needing its services than there are beds. So they’re often taken to regular emergency rooms for stabilization or because they also have medical issues that need to be addressed.
That sometimes means other patients — with strokes, heart attacks or injuries — must wait, Tcheng said.
“Someone coming in three and four times a day takes a toll on the system,” he said. “It’s incredibly dispiriting.”
He compared the fight against San Francisco’s threefold crisis — a lack of housing, mental health care and drug treatment — to building a three-legged stool. Addressing just one or two legs won’t work.
Tcheng, a 36-year-old Potrero Hill resident, works in four emergency rooms around the city, but couldn’t get permission from his bosses to name them. But really, they’re interchangeable — each one flooded daily with unsheltered patients suffering from psychosis who need treatment but aren’t getting it.
Rachel Rodriguez, a social worker in another emergency room in the city, confirmed the crisis exists at her hospital, too. She couldn’t talk for a while Tuesday because, as she texted, her ER was “bursting” with psychiatric patients. She said social workers are so strapped caring for psychiatric patients that they often can’t provide help to others who need it — such as domestic violence victims or those hurt in car crashes.
She has started emailing the Department of Public Health every day with a tally of the people waiting for acute psychiatric beds in her hospital alone. One email from last month showed 15 patients ranging in age from 21 to 86, a few waiting a month or longer.
Rodriguez said she’s reserving judgment about Newsom’s plan. But her husband, Charlie Berman, a clinical social worker in San Francisco, said he fears it’s nothing more than “a political facade masking the ineffectuality of a rotten system,” and called the city’s emergency rooms “extensions of the Tenderloin with ambulances providing taxi service in between.”
Berman said the governor’s plan will fail without a major investment in locked psychiatric wards and beds designed for people with both mental illness and substance use disorder. Both are very expensive.
Tcheng is more hopeful — provided the governor finds the money to pay for treatment through CARE Court. Civil libertarians are already speaking out against the plan, saying that mandating care is inhumane and not as effective as providing voluntary services, but Tcheng said the real inhumanity is playing out in the city’s emergency rooms every day.
“I fundamentally reject the notion it’s more compassionate to let these people live on the streets and die in alleyways than to mandate that they get care,” Tcheng said. “I just think it’s appalling what San Francisco has allowed to happen to some of these patients.”
He cited Mary Botts, the San Francisco homeless woman dubbed “Princess Leia” for often wearing her hair in buns on the sides of her head, sometimes held together with syringes. She frequently walked into traffic at Castro and Market streets and slept in the gutter.
Tcheng said he treated her at least a dozen times — but kept releasing her back to the streets because she didn’t want help and there was nowhere to send her. She died of a drug overdose in November 2020 at age 28.
At a Board of Supervisors hearing last week, Superior Court Judge Michael Begert addressed the severe shortage of treatment beds. He oversees drug court, which aims to clear defendants’ arrests if they can prove they’ve successfully addressed the drug problem that led them to commit the crime. Begert said he has never been able to access a treatment bed for somebody who allegedly committed a crime and suffers from both mental illness and a drug addiction. Instead, such people often linger in jail — with one person waiting 264 days behind bars for a bed — until they’re eventually released, having further deteriorated while jailed.
“This is not treatment on demand, and they’ve been talking about treatment on demand for at least 25 years,” Begert said.
Two years ago, the Department of Public Health released a study stating the city needs 400 more treatment beds, but it’s added only 89 beds since then. And even 400 might not be enough, said Supervisor Hillary Ronen. She said the board hearing left her with “a mix of exasperation, sadness, frustration, but also a new resolve” to vastly improve the city’s mental health system.
Ronen said she doesn’t know enough about CARE Court to form an opinion, but hopes it’s not another “shiny new program” from a politician wanting to look good.
For now, Tcheng will keep seeing the same patients in his ER, and many will leave no better off than when they arrived. The man who tried to steal the submarine got released after he slept off his high. Tcheng doesn’t know what happened to him after that.
As for the man who ate a raccoon?
Tcheng said he asked a psychiatrist to evaluate whether he should be treated under an involuntary hold. But, he said, the man wasn’t deemed to fit the requirement of being “gravely disabled” under state law if he could secure his own food. Even if that food was roadkill.
Tcheng said he managed to get a different doctor to test the man for rabies, but he lost track of him after that.
“Hopefully, he got some sort of psychiatric care,” Tcheng said. “But knowing San Francisco, I doubt it.”
San Francisco Chronicle columnist Heather Knight appears Sundays and Wednesdays. Email: hknight@sfchronicle.com Twitter: @hknightsf
Dr. Scott Tcheng is an emergency room physician at several San Francisco hospitals.
Photo: Carlos Avila Gonzalez/The Chronicle