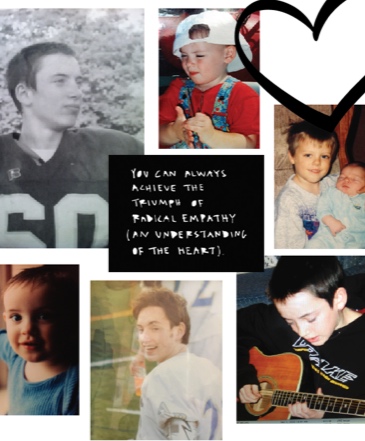
Jared was my second son born into our family of two boys in 1991. He was a quiet child, deeply intuitive and sensitive, musically gifted, and athletic. A boy full of life and funny faces and stories. He always made us laugh. Our Jared.
As he approached his junior year in high school, life began to take twists and turns that led us to seek help. The hope was always that help was just an appointment away. Then, as Jared became an adult at the ripe old age of 18, privacy laws separated us. I was behind an immovable glass wall, unable to reach him. HIPAA stood guard like a heartless warden of his declining mental health. The nightmare began, and evolved into multiple chapters of heart-wrenching sadness, agonizing decisions, and defeating barriers.
March 12, 2018: My boy needs continuous prayers. He’s been in a group home for three years. I had to make him homeless in order to make him eligible for residential support. He spent seven months in a respite bed, above an overdose crisis lock-up treatment center in the worst area of Worcester, Massachusetts, waiting for a bed in a group home.
This past year, Jared grew more depressed over his circumstances and wanted desperately to return home. He began self medicating with alcohol. The house set up a protocol to call an ambulance if they believed he was intoxicated. The ambulance brought the police and, because Jared suffers from paranoia and schizophrenia, he didn’t believe the police were real police. They grabbed him, he pulled back, and they proceeded to beat the daylights out of him. They beat him so badly he had to be taken to the hospital.
North Hallway, Position 8 — A bed with a confused, hungry, and lost young man could be found in that hallway on a gurney. His illness, schizophrenia, was treated like a crime. His ride to the hospital began with a knee pressing into his neck, and tight cold wrings that left behind purple shadows of remembrance on both wrists. He was surrounded by at least six or seven other hallway-mates. They also bore the markings of a war-torn life battling the disease that we treat as dirty. I saw dirty hair, dirty clothes, and listened to dirty mouths. Whispering and cries were the audible clues they were suffering. No one was offered a drink of water. I observed avoidance. Did I detect annoyance?
Twenty long hours in that hallway waiting for the next step. This was a crisis — so many in need and so few helpers and healers. I was there for him, but no one showed up for any of the others. The lost and neglected souls of the North Hallway.
After the hospital, Jared was locked up at a Worcester police station and bail was posted. He had to appear in court to be charged with assault on police. When he arrived at court, they put him in lock-up all day. The judge heard his case at 4:30 p.m. He ruled that Jared was a danger to himself (drinking) and others (resisting police). They sent him to a Plymouth, Massachusetts, correctional facility for a mandatory 90-day rehab. This rehab required that he live in a cell, wear an orange jumpsuit, and be treated like a criminal.
My son tried calling me, yesterday, and it took four minutes to set up an account to pre-pay $1 per-minute to talk to him. By the time I did that, he’d hung up. I could barely breathe.
The grief and feelings of helplessness are indescribable. The mentally ill are so drastically mistreated and misunderstood. There are no beds available in genuine rehab places because of the opioid crisis. The only places left are correctional facilities.
Distress worsens mental illness. Mental health care is a system built on failure and supported by a nation that stigmatizes mental illness. It’s only recently recognized that we’re still in the dark ages when it comes to treating diseases of the brain.
January 19, 2019: Jared was just released from a 40-day imprisonment at a house of correction followed by a 35-day inpatient hospitalization at a state hospital. He had a psychotic break in late October while visiting me for a few days. He believed I was part of the KKK and pulled a kitchen knife out of the knife rack. He didn’t hold the knife up to me and I never saw what kind of knife he pulled. I called for help, reluctantly, because we had just had a three-year case dismissed for assault and battery on a police officer because he resisted them last time I called them.
The local police called in what is a called a STOP team, which I would classify as a SWAT team. Heavily armed men unloaded from vans and surrounded our house. They appointed me the negotiator and hooked me up to a speaker inside the house while a robot took photos inside the house. My small dog was inside with Jared. It was cold and raining. Every 45 minutes I had to stand three feet away from two men holding automatic weapons and one holding a shield and a taser. I was shaking like a leaf. I was luring my son into a trap. If he did anything threatening, I feared he’d be blown to pieces. Team members were in the woods, too. I could see little red lights coming from their weapons and helmets — a scene from Star Wars. The Ewoks in the woods. They evacuated my neighbors. It was insane.
After an eight-hour stand off, the police smashed a battering ram through Jared’s particle-board bedroom door that didn't have a lock, destroyed his room, stepped on his guitar, and arrested him. They charged him with attempted murder among three other trumped up charges.
I started a Go Fund Me campaign and borrowed money from my family to pay for a private attorney. The court appointed attorney was definitely not paying attention and cared very little about Jared's rights.
The local newspaper wrote a story that made my son sound like a terrorist — I believe to justify the manpower that was brought to the neighborhood. Over 25 state police cruisers, 2 local police departments, and an ambulance surrounded my home and lined my street. I wrote to the paper and asked to tell my side of the incident. They featured me and my story on the cover on the Sunday edition.
Jared’s back at the group home. He’s stable. They’re working with him to keep him busy and going to therapy and AA. I saw him yesterday. He was cleaning his room, lining up his shoes, hanging up his clothes, and tolerating my visit. In the past, he wouldn't want me in his space. This is progress.
Every day is a gift. I believe in God and the power of prayer.