My son, James, is 34. I'm so proud of the man he's become, and grateful to everyone who's helped him get where he is today. Mostly though, I'm grateful for him.
You see, although I'd take away his illness if I could, his journey's made me a better person. Although I'd eliminate all the pain he's walked through, his pain's enabled me to be more compassionate. Although I'd give him back the life he knew before his symptoms took it all away, I'm grateful each day that he is alive and able to give and receive love.
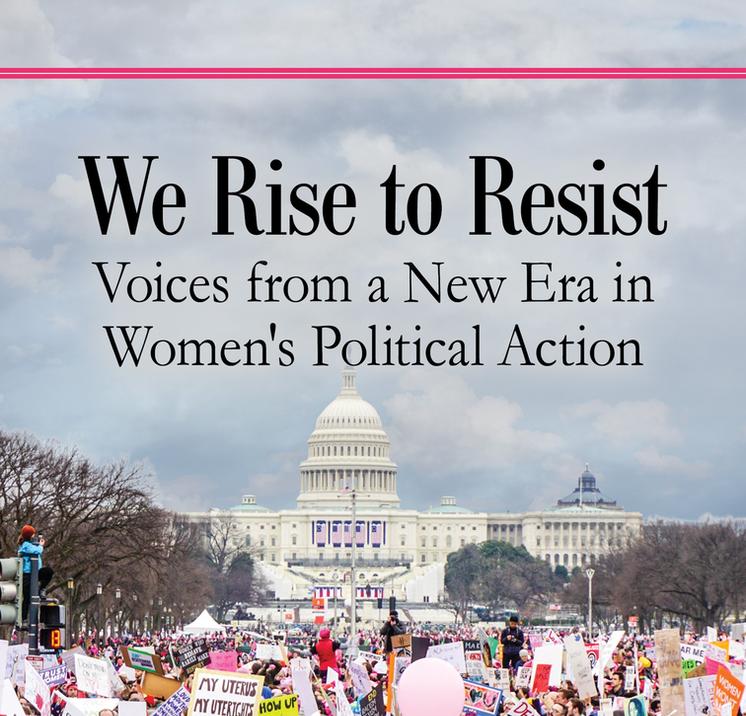
This picture was taken in January 2017. James looks the same except that he's thinner now. There were so many times along the way that I never, in my wildest dreams, thought he could enjoy such a wonderful quality of life. Don't get me wrong, he can't hold a full time job and will never be totally independent, but he's accomplished so much more than we dared to hope for.
James
A wise man once told me that what I needed to do was give my son something he didn't want to loose. This was what I built everything on. It's a solid foundation. Of course, as you well know, doing it takes a village!
Just a little back story because I understand how hopeless and overwhelming caregiving for our loved ones can be — the pain, the endless stress, the blocked paths to treatment, the grief, and the feeling of isolation. For my son, his journey started before his birth, really. I was high risk due to having placenta previa and he was in fetal distress during labor. They couldn't find a vein for an IV so I could have a C-section so other methods had to be used. James was blue from a knot in the umbilical cord that was wrapped around his neck.
When James was in second grade, he was diagnosed with ADHD and we started behavior modifications along with medication. He continued with behavior modifications until he became so ill that they didn't work well.
James was always a gifted athlete. In his freshman year of high school, his coaches told him to look for college scholarships in basketball, baseball, and football. But, by age 15, his symptoms were severe and he was put in a locked down facility out of state because he was still a minor. I appealed to the court to release him into my care so I could get him treatment. He needed treatment, not punishment, and it's in the right treatment that we found our hope. That's why I do what I'm able to help more find their treatment in time.
My son's been and continues to be one of my greatest blessings and the best teacher I've ever had. I'm honored to know him and to have the privilege of being his mom. At long last, he's at peace with his life. He's on the other side of his horrific journey. His kindness, gentleness, and his never giving up have lead him here. He's able to enjoy the present and let go of what once was.